Types of face coverings (masks) and coronavirus disease 2019 (COVID-19)
Abstract
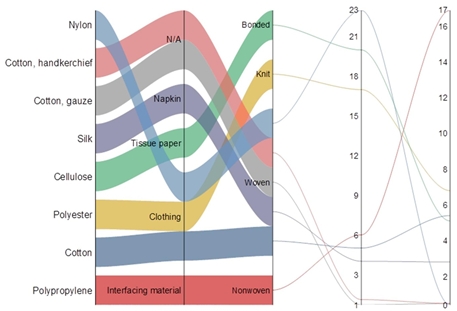
The ongoing pandemic has been increasing slowly and steadily across the world. The SARS-CoV-2 spreads through droplet disseminated from infected persons via coughing and/or sneezing onto the face, nasopharyngeal, and oropharyngeal mucosa. In order to prevent the transmission of coronavirus disease, WHO and public health officials made policies, advised the health workers and public to wear face coverings (masks). The nature of masks depends upon the source, material, structure and particulate efficacies. The main objective of this study is to provide information about efficacies of different types of masks used during COVID-19 pandemic.
Downloads
References
2. Islam T, Magray JA, Zargar SA. Role of Herbs against COVID-19. Hospitality and Tourism Industry amid COVID-19 Pandemic, 409.
3. Zargar SA, Islam T, Rehman IU, Pandey D. Use of Cluster Analysis To Monitor Novel Corona Virus (Covid-19) Infections In India. Asian J Adv Med Sci. 2021: 1-7.
4. Pandey D, Islam T, Malik MA. Novel Coronavirus Disease (Sars-Cov-2): An Overview. Asian J Adv Med Sci. 2021: 8-12.
5. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med. 2020; 382(18): 1708-1720.
6. Giovanetti M, Benvenuto D, Angeletti S, Ciccozzi M. The first two cases of 2019‐nCoV in Italy: Where they come from? J Med Virol. 2020; 92(5): 518-521.
7. Rather RA, Islam T, Rehman IU, Pandey D. Development of vaccine against coronavirus disease 2019 (Covid-19) In India. Asian J Adv Med Sci. 2021: 13-21.
8. Pandey D, Islam T, Magray JA, Gulzar A, Zargar SA. Use of statistical analysis to monitor novel coronavirus-19 cases in Jammu and Kashmir, India. Eur J Biol Res. 2021; 11(3): 274-282.
9. Liu J, Zheng X, Tong Q, Li W, Wang B, Sutter K, et al. Overlapping and discrete aspects of the pathology and pathogenesis of the emerging human pathogenic coronaviruses SARS‐CoV, MERS‐CoV, and 2019‐nCoV. J Med Virol. 2020; 92(5): 491-494.
10. Center for Disease Control. Strategies for optimizing the supply of N95 respirators: crisis/alternate strategies. https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/crisis-alternate-strategies.html (Accessed February 22, 2021).
11. Center for Disease Control. Recommended guidance for extended use and limited reuse of N95 filtering facepiece respirators in healthcare settings. https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html#risksextended (Accessed February 24, 2021).
12. Bárcena M, Oostergetel GT, Bartelink W, Faas FG, Verkleij A, Rottier PJ, Bosch BJ. Cryo-electron tomography of mouse hepatitis virus: insights into the structure of the coronavirion. Proc Nat Acad Sci. 2009; 106(2): 582-587.
13. Neuman BW, Adair BD, Yoshioka C, Quispe JD, Orca G, Kuhn P, Buchmeier MJ. Supramolecular architecture of severe acute respiratory syndrome coronavirus revealed by electron cryomicroscopy. J Virol. 2006; 80(16): 7918-7928.
14. Qian Y, Willeke K, Grinshpun SA, Donnelly J, Coffey CC. Performance of N95 respirators: filtration efficiency for airborne microbial and inert particles. Am Ind Hyg Assoc J. 1998; 59(2): 128-132.
15. Lee SA, Grinshpun SA, Reponen T. Respiratory performance offered by N95 respirators and surgical masks: human subject evaluation with NaCl aerosol representing bacterial and viral particle size range. Ann Occup Hyg. 2008; 52(3): 177-185.
16. Bałazy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, Grinshpun SA. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control. 2006; 34(2): 51-57.
17. European Standards. UNE EN 14683:2019+AC:2019. Medical Face Masks-Requirements and Test Methods. 2019; https://www.en-standard.eu/une-en-14683-2019-ac2019-medical-face-masks-requirements-and-test-methods/ (Accessed February 18, 2021).
18. F23 Committee, n.d. Specification for Performance of Materials Used in Medical Face Masks. ASTM International. (https://doi.org/10.1520/F2100-19E01 (Accessed February 16, 2021).
19. Dato VM, Hostler D, Hahn ME. Simple respiratory mask: simple respiratory mask. Emerg Infect Dis. 2006; 12(6): 1033.
20. Rengasamy S, Eimer B, Shaffer RE. Simple respiratory protection - evaluation of the filtration performance of cloth masks and common fabric materials against 20–1000 nm size particles. Ann Occup Hyg. 2010; 54(7): 789-798.
21. Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013; 9(3): e1003205.
22. Jeffus L. Welding and metal fabrication. Cengage Learning. 2011.
23. Jung H, Kim JK, Lee S, Lee J, Kim J, Tsai P, et al., Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual Res. 2013; 14(3): 991-1002.
24. Taupin JM, Cwiklik C. Scientific protocols for forensic examination of clothing. CRC Press. 2010.
25. Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano 2020; 14(5): 6339-6347.
26. Bandini C, Sabatini I, Dimilta M, Baldessari G. Basic Characteristics of Antipollution Devices and PPE. In Clinical Handbook of Air Pollution-Related Diseases. Springer, Cham. 2018: 543-566.
27. Hubbard BR, Pearce JM. Conversion of self-contained breathing apparatus mask to open source powered air-purifying particulate respirator for fire fighter COVID-19 response. HardwareX. 2020; 8: e00129.
28. World Health Organization. Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020. No. WHO/2019-nCoV/IPC_Masks/2020.
29. Christie CD, Glover AM, Willke MJ, Marx ML, Reising SF, Hutchinson NM. Containment of pertussis in the regional pediatric hospital during the Greater Cincinnati epidemic of 1993. Infect Control Hosp Epidemiol. 1995; 16(10): 556-563.
30. Huston P, Hogg W, Martin C, Soto E, Newbury A. A process evaluation of an intervention to improve respiratory infection control practices in family physician offices. Can J Public Health. 2006; 97(6): 475-479.
31. Loeb M, McGeer A, Henry B, Ofner M, Rose D, Hlywka T, et al. SARS among critical care nurses, Toronto. Emerg Infect Dis. 2004; 10(2): 251.
32. Inouye S, Matsudaira Y, Sugihara Y. Masks for influenza patients: measurement of airflow from the mouth. Jpn J Infect Dis. 2006; 59(3): 179.
33. Ki HK, Han SK, Son JS, Park SO. Risk of transmission via medical employees and importance of routine infection-prevention policy in a nosocomial outbreak of Middle East respiratory syndrome (MERS): a descriptive analysis from a tertiary care hospital in South Korea. BMC Pulm Med. 2019; 19(1): 1-12.
34. Laosiritaworn Y. Computational modeling to address the burden of influenza and strategies of control measures in Thailand (Doctoral dissertation, University of Pittsburgh). 2014.
35. Kim T, Jung J, Kim SM, Seo DW, Lee YS, Kim WY, et al. Transmission among healthcare worker contacts with a Middle East respiratory syndrome patient in a single Korean centre. Clin Microbiol Infect. 2016; 22(2): e11-e13.
36. MacIntyre CR, Cauchemez S, Dwyer DE, Seale H, Cheung P, Browne G, et al. Face mask use and control of respiratory virus transmission in households. Emerg Infect Dis. 2009; 15(2): 233.
37. MacIntyre CR, Wang Q, Seale H, Yang P, Shi W, Gao Z, et al. A randomized clinical trial of three options for N95 respirators and medical masks in health workers. Am J Respir Crit Care Med. 2013; 187(9): 960-966.
38. MacIntyre CR, Chughtai AA, Rahman B, Peng Y, Zhang Y, Seale H, et al. The efficacy of medical masks and respirators against respiratory infection in healthcare workers. Influenza Respir Vir. 2017; 11(6): 511-517.
39. MacIntyre CR, Seal H, Dung TC, Hien NT, Nga PT, Chughtai AA, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open, 2015; 5(4): e006577.
40. Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin Infect Dis. 2017; 65(11), 1934-1942.
41. Seto WH, Tsang D, Yung RWH, Ching TY, Ng TK, Ho M, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet. 2003; 361(9368): 1519-1520.

This work is licensed under a Creative Commons Attribution 4.0 International License.